We have all heard about people having to travel miles, often on foot to access medical care in rural India. Some of them don’t get access to proper treatment on time, others lose their lives. Just think about this. According to the 2011 Census of India, approximately 70% of the Indian population lives in rural areas. But many of these areas lack adequate healthcare infrastructure, and people in these regions often have to travel long distances to access medical facilities. Even then, they may not be able to meet specialists. That’s where mobile health units or healthcare on wheels initiatives play a vital role as they help screen, diagnose, and treat people at their doorsteps.
Majority of rural Indians do not have access to healthcare
Bharat Health Index (BHI) 2023 survey shows that only 25% of the semi-rural and rural population in India have access to modern healthcare facilities within their localities. The accessibility index saw a major dip as one moved from urban to rural India, with only 10% of the rural respondents citing that they had access to healthcare within a 10km radius.
The lack of skilled healthcare providers at the last mile poses a significant challenge to accessibility. Only 15% respondents confirmed having a doctor’s clinic or healthcare facility within a 5km radius. While 25% had access to general physicians in their area, 92% lacked specialists, such as cardiologists, gynaecologists or paediatricians impacting medical care.
Advantages of using mobile healthcare units
“Accessing healthcare services is a problem in rural areas, and reaching out to specialists is difficult. It’s even more challenging if the patient is not mobile, physically challenged, visually or hearing impaired as then getting out of the home to access health services is an issue. Often, they have to travel 10-15 km to reach the nearest medical facility,” says Dr Sridhar Vaitheeswaran, consultant psychiatrist, SCARF, who has been in charge of a mental health programme in Chengalpattu, Tamil Nadu, which helps rural people access mental healthcare.
Another problem is the fact that many older adults live alone as their family members have migrated to other places. “So they are unable to access these services,” he says.
Yet another issue is the lack of availability of all medicines and facilities in local healthcare centres. Many investigations that need to be done or special medicines may not be available locally and mobile healthcare services help bridge this gap.
These mobile clinics reach areas that lack proper medical infrastructure and provide basic healthcare services, such as consultations, preventive care, immunizations, maternal and child healthcare, and diagnostic tests, making it easier for people to access medical help.
In some cases, mobile healthcare units are equipped to provide emergency medical services and may even have specialists or equipment onboard to treat certain conditions that may otherwise require patients to travel to urban centres.
It also helps early detection and treatment of diseases. “We have had young people in their late 20s walk in and found that they have high BP and sugar levels. These are people at high risk of having a stroke or heart attack who don’t even realise that they have these health issues as they don’t have any symptoms,” says Dr V Mohan, chairman, Dr Mohan’s Diabetes Specialities Centre, Chennai, whose team works with the Sri Sathya Sai Seva Organisation (SSSSO) to operate free mobile clinics.
Healthcare on wheels helps reduce transportation costs for people in rural areas as travelling to a distant healthcare facility can be both expensive and time-consuming. Many of these services also include educational programmes that inform rural populations about health issues, hygiene practices, disease prevention, and healthy lifestyles, which can have long-term benefits on community health.
Maternal and child health is one area where mobile clinics play a vital role, providing prenatal and postnatal care, vaccination services, and basic check-ups, helping to reduce maternal and infant mortality rates in rural areas.
Regular visits by mobile healthcare units allow for ongoing monitoring of chronic diseases like diabetes, hypertension, and infections, ensuring that rural populations receive the follow-up care they need. By offering services to rural populations, healthcare on wheels helps reduce the burden on already overcrowded urban hospitals and clinics.
Government initiatives help deliver healthcare to the doorstep
The Indian government has launched several initiatives to provide healthcare on wheels, particularly to address the challenges of delivering healthcare services to remote and underserved rural areas. These initiatives aim to bridge the gap in healthcare access and ensure that rural populations can receive essential medical services.
For instance, under the National Health Mission (NHM), which encompasses the National Rural Health Mission and the National Urban Health Mission, the government provides funding and support to states to establish mobile medical units (MMUs) in rural areas. These units offer regular health check-ups, treatment for common ailments, maternal and child health services, vaccination campaigns, and prevention of diseases like malaria and tuberculosis. Various states, such as Rajasthan, Uttar Pradesh, Madhya Pradesh, and Odisha, have implemented mobile health units under this programme.
As part of Ayushman Bharat, the government has launched Health and Wellness Centers (HWCs) to offer comprehensive healthcare services to rural populations. While many of these centers are stationary, there are mobile health units that complement the HWCs. Apart from the regular healthcare services, these units also offer essential diagnostic and laboratory services.
Several states have implemented their own mobile healthcare programmes to improve access to healthcare for rural populations. The Tamil Nadu government’s flagship programme, Makkalai Thedi Maruthuvam Scheme, offers a comprehensive set of home-based health care services to ensure a continuum of care and meet the health needs of beneficiaries in the family.
“It’s very innovative and doing well so the need for us conducting these camps is much less nowadays,” says Dr Mohan, adding that Tamil Nadu also won the ‘United Nations Interagency Task Force Awards (UNIATF) for 2024’ for the programme.
Private initiatives also help
Many initiatives rope in the local community, and have volunteers and community level workers who have been trained to screen people for mental health issues and to refer them to psychiatrists.
NGOs play a vital role
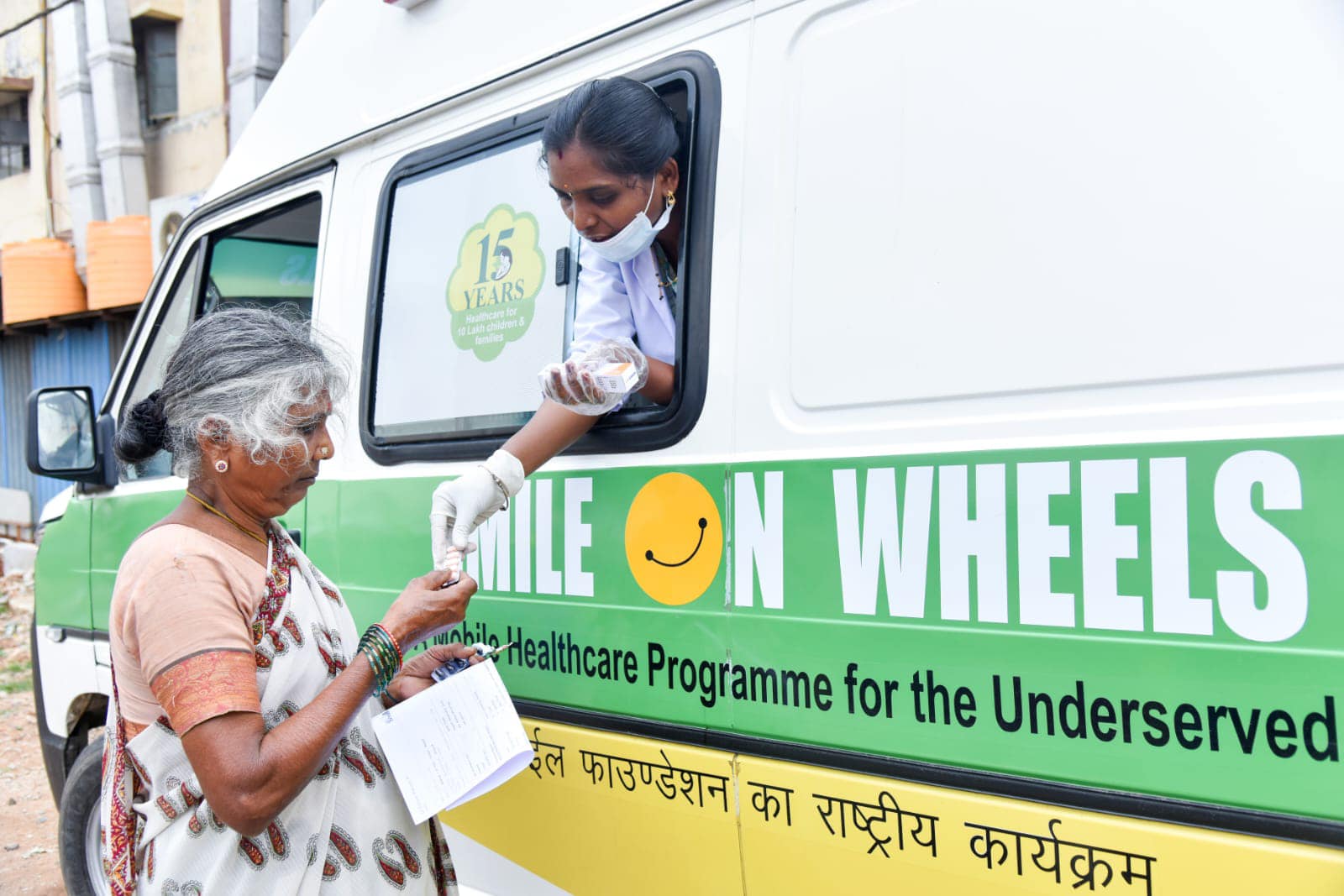
NGOs have also launched mobile units to help with delivery of healthcare services to rural areas. Smile Foundation’s healthcare intervention provides primary healthcare facilities at the doorsteps of the underserved communities in identified rural areas and urban slums. The aim is to reach the vulnerable population who cannot afford basic healthcare facilities.
Our Smile on Wheels (SoW) programme aims to reach the unreached through fully-equipped Mobile Healthcare Units staffed with doctors and paramedics, providing OPD services, point-of-care test facilities and medicines.
To make dental treatment affordable and accessible and to address the gaps existing in dental healthcare at the community level Smile Foundation joined hands with GlaxoSmithKline Asia Private Limited (now Haleon). The dental health units have been providing diagnostic as well as curative services through roster based OPDs. They organize regular Information, Education and Communication (IEC) activities to enhance health seeking behaviour.
Another very important component of the Smile on Wheels Dental HealthCare is the School Oral Health Programme that includes awareness sessions on oral health and hygiene followed by regular dental check-ups.
Our interventions in Tamil Nadu and Karnataka
SoWs has made a tremendous impact on the health of the community in Indalawadi village, nestled in the remote Anekal block on the border of Tamil Nadu and Karnataka, which has faced numerous challenges in accessing healthcare services.
The village is home to around 1,230 residents, the majority of whom are farmers and daily wage workers with limited financial resources. The high transportation costs required to travel to Anekal Government Hospital posed a substantial obstacle for the community in accessing crucial healthcare services.
SoW’s mobile clinic has provided a total of 1,881 consultations, catering to the diverse healthcare needs of the villagers. 76% of these consultations were for females and children, highlighting the importance of accessible healthcare for vulnerable populations.
During these consultations, approximately 18% of the patients were diagnosed with Hypertension and Diabetes Mellitus II, requiring regular check-ups and medication. SoW has played a crucial role in monitoring their blood pressure and sugar levels, ensuring that these patients receive the necessary care and support. Through timely treatment and regular monitoring, the initiative has significantly improved the health outcomes of community members living with these conditions.